Dermoid cysts are the most common congenital lesions of the orbit. They
are developmental choristomatous tumors which are defined as normal tissue in
an abnormal location. They are composed of derivatives of epithelial or
connective tissue elements that are entrapped within facial clefts during
embryogenesis, or from failure of separation of surface ectoderm from the
neural tube. The solid or cystic masses are formed by proliferation of these
cells1. They represent 24% of all orbital and eyelid masses, 6 – 8
of deep orbital tumors and 80% of cystic orbital masses2. Conjunctival
dermoid cysts are solid choristomas2, typically unilateral and
located at the infertemporal limbus.
They are well – defined slow growing painless lesions and have local
mass effect on the bone with erosion and remodeling. Growth may be outward into
the eyelid, noted typically in childhood, or inward into the orbital cavity,
and hence presents later. Although congenital, only one fourth lesions are
clinically obvious at birth, the remaining presenting within the first year.
Occasionally they present acutely after rupture simulating an acute
inflammation with erythema, tenderness and swelling due to leakage of keratin3.
Mostly, dermoid
cysts arise from keratinized squamous epithelium, but they may occasionally
originate from the nonkeratinized conjunctival epithelium4. Treatment
is complete surgical excision, following which recurrences are rare. The purpose
of our study is to segregate dermoids according to their site and to manage
them diagnostically and surgically using different surgical approaches and to
evaluate the results.
MATERIAL AND
METHODS
All patients with dermoid cysts presented to the ophthalmology department
at
All limbal dermoids were superficial and removed by shave excision and
conjunctival autografting or a sliding flap. The superficial medial orbital
dermoids were excised via medial skin incision or fronto-ethmoidal (Lynch)
incision. The superficial lateral dermoids were removed by sub-brow incisions.
Deep orbital dermoids were removed with a lateral orbitotomy in six (6) cases
and Lynch medial orbitotomy in one (1) case. In ten (10) cases, drainage was
considered necessary before total removal. Follow-up ranged from one month to
four years and there was no recurrence seen.
RESULTS
A total of 28 cases were diagnosed and treated, out of which 12 (42.9%)
were limbal dermoids. Seven (25%) were superficial orbital, out of which 5 were
medial (supero-nasal) orbital related to the frontoethmoidal suture and 2 were
lateral (supero-temporal) orbital related to the zygomaticofrontal suture. Nine
(32%) were deep orbital, out of which 5 were related to the zygomatico-frontal
suture, one superior orbital fissure,
one posterior ethmoido-sphenoidal suture and 2 were related to the trochlear
fossa (Table 1) (Fig. 1).
Table 1. Location of Dermoid
|
Location |
Frequency n ( %) |
|
Inferotemporal |
12 (42.9) |
|
Superotemporal |
8 (28.6) |
|
Superonasal |
6 (21.4) |
|
Temporal |
2 (7.1) |
|
Total |
28 (100) |
Limbal dermoids were all superficial and located on the inferotemporal
limbus. Removal resulted in mild corneal thinning and scarring, but no lesion
required keratoplasty. One case was diagnosed as Goldenhar syndrome.
Superficial medial and lateral dermoid cysts were present below the
brow. Rupture occurred in four (4) cases and the area was irrigated with saline
and a dilute steroid solution. There was one case of recurrent superficial
lateral dermoid which was treated successfully. Deep orbital cysts were
difficult to excise with drainage being considered necessary to facilitate
posterior wall removal. No significant postoperative inflammation was observed
in any case.
All cysts were completely removed and sent for histopathology. They
were found to be lined with stratified squamous epithelium, filled with
keratin, sebaceous material and hair.
Patients were
followed up for one month to four years to check for recurrences. One (1)
patient developed a peri-ocular hematoma which spontaneously resolved.
DISCUSSION
Solid limbal dermoids are usually unilateral pale lesions2
located most commonly at the inferotemporal limbus. Mostly they are superficial
and deep extension into cornea, sclera and conjunctiva is a rarity. Treatment
is shave excision, while lamellar or penetrating keratoplasty may be needed for
deeper extension. Bilateral limbal dermoids are found in patients with
Goldenhar’s syndrome.
Orbital dermoids can present at any age from infancy to old age. A slow
growing, painless, subcutaneous mass presents in 90% of cases. They are
non-tender, fluctuant or firm, and enlarge slowly as they become filled with
keratin and sebum. Deeper lesions usually symptomless initially, present later
in life, in early adolescence or adulthood. Deep dermoids if enlarge
sufficiently may result in proptosis, diplopia due to globe compression or
motility restriction due to cranial nerve palsies (III, IV or VI)3.
Decreased vision due to optic nerve compression is rare. Rarer still is its
location within a rectus muscle5. They are usually unilateral with
no predilection for laterality, gender or race.
In our study, limbal dermoids were greatest in frequency, followed by
deep orbital dermoids and lastly, superficial dermoids. We found superficial
orbital demoids predominantly superonasally, however Cavazza et al6
in their study, found predominantly superotemporal dermoids and Sherman7
et al found equal number of medial and lateral dermoids in their study. Deep dermoids were mostly lateral in our study. Dermoids occur along
the superotemporal orbital margin at the zygomatico-frontal suture
in 75% of cases, although the fronto-ethmoidal suture, superonasally is the
next most common site5. Other sites are frontonasal and
frontolacrimal sutures.
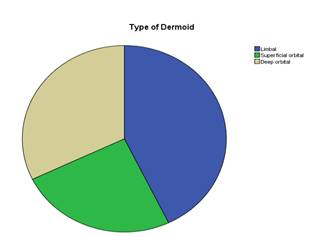
Fig. 1: Pie chart depicting percentages of types of Dermoid

Fig. 2. A large left
recurrent superficial orbital dermoid cyst
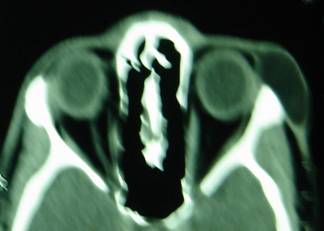
Fig. 3:
CT scan depicting the same cyst

Fig. 4: Postoperative
appearance at 3 weeks after excision
Dermoids are classified clinically into superficial or deep dermoids or
exophyic and endophytic, according to
their site of attachment in relation to the orbital rims8. Superficial dermoids lie subcutaneously anterior to the orbital
septum and their posterior margins can be palpated easily. Deep lesions are
located posterior to the orbital septum within the orbital cavity, discovered
later in life when they produce bone damage, with or without invasion of the adjacent
structures. Deep dermoids are often complicated and may be misdiagnosed due to
extent and complexity. In
order to distinguish between deep and superficial dermoids, a thorough
investigation is necessary, since deep dermoids may extend beyond the orbit
into the temporalis fossa or intracranially9. Also significant is
the recognition of size, character, extension, and bony defects.
Histopathologically, dermoids are lined with keratinized, stratified,
squamous epithelium with dermal appendages like hair follicles, sebaceous and
eccrine glands and filled with keratin and sebaceous secretions. Rupture leads
to intense inflammation mimicking orbital cellulitis. Histological evidence of
leakage with inflammation has been found in more than half of these lesions10.
Ultrasonography
reveals irregular internal structure on A-scan, with low to medium internal
reflectivity, with the cyst wall being highly reflective. B-scan shows these
lesions as round, smooth and well-defined with variable internal appearance11
and occasional fluid levels. Excavation of adjacent bone or defects are
frequent.
Management of dermoid cysts is complete surgical excision of the cyst
wall and contents. Most lesions show leakage and
associated inflammation on histopathology. The risk of rupture increases with
patient age and size of the cyst12, due to thinning of the wall with
increased size and also increased risk of trauma with age. Therefore, these
should be removed early to prevent tissue fibrosis. The superficial lesions are
managed by a direct approach over them with. An upper-eyelid incision provides
adequate exposure of most orbital lesions13.
Recognition
of clinical features and imaging findings of dermoids is essential and with the
help of imaging examinations and the combination of various surgical skills,
the recurrence of dermoid cysts can be effectively prevented.
CONCLUSION
To conclude, we
clinically evaluated dermoid cysts which presented to us, calculated their frequency
and investigated them with CT scanning/ MRI and managed them surgically and
confirmed via histopathology. Enbloc dissection is the best method to remove
these cysts with minimal complications.
Author’s affiliation
Dr.
Sana Nadeem
Senior
Registrar
Department
of Ophthalmology
Dr.
Ali Raza
Associate
Professor
Head
of Ophthalmology Department
REFERENCE
1.
Apple DJ, Rabb MF. Ocular Pathology. Fifth edition. Mosby:
2.
Yanoff M, Duker JS. Ophthalmology. Second Edition. Mosby:
3.
Karcioğlu ZA. Orbital tumors: diagnosis and treatment.
Springerlink:
4.
Dutton JJ, Fowler AM,
Proia AD. Dermoid cyst of conjunctival origin. Ophthal Plast Reconstr Surg.
2006; 22: 137-9.
5.
Howard GR, Nerad JA, Bonavolonta G, et al. Orbital dermoid cysts located within the lateral rectus muscle. Opthalmology. 1994; 101: 767-71.
6.
Cavazza S, Laffi GL, Lodi L, et al. Orbital dermoid cyst of childhood: clinical pathologic findings,
classification and management. Int Ophthalmol. 2011; 31: 93-7.
7.
8.
Bonavolontà G, Tranfa F, de Conciliis C, et al. Dermoid
cysts: 16-year survey. Ophthal Plast Reconstr Surg. 1995; 11: 187-92.
9.
Pfeiffer RL, Nicholl RJ.
Dermoid and epidermoid tumours of the orbit. Arch Ophthalmol. 1948; 40: 639.
10.
Shields JA, Kaden IH, Eagle RC Jr,
et al. Orbital dermoid
cysts: clinicopathologic correlations, classification, and management. The 1997
Josephine E.
11.
Schuleler
lecture. Ophthal Plast Reconstr Surg. 1997; 13: 265-76.
12.
Traboulsi EI, Azar DT, Khattar J, et al. A-scan ultrasonography in the diagnosis of
orbital dermoid cysts. Ann Ophthalmol. 1988; 20: 229-32.
13.
Colombo F, Holbach LM, Naumann GO. Chronic
inflammation in dermoid cysts: a clinicopathologic study of 115 patients. Orbit. 2000; 19: 97-107.
14.